General Orthopedics
Knee Arthritis
There are many different types of arthritis that can affect the knee, but the most common ones are osteoarthritis, rheumatoid, and post-traumatic arthritis.
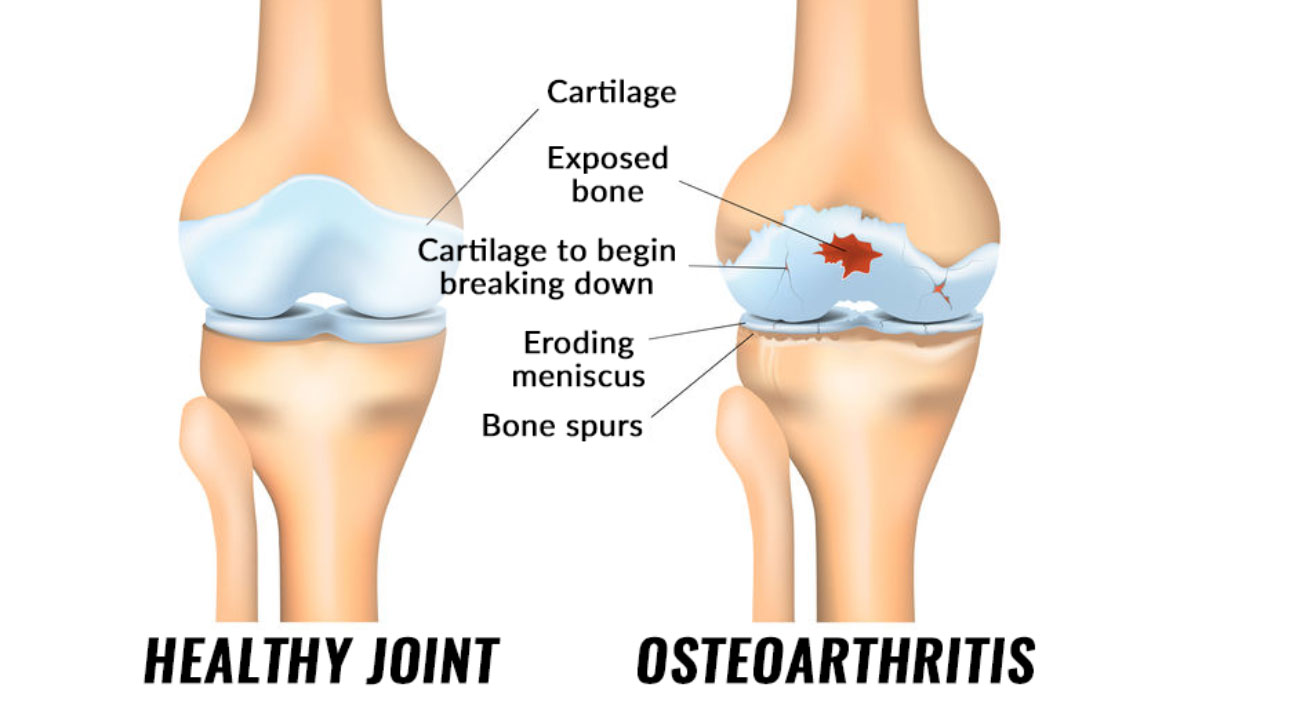
The knee joint is the largest joint in your body. It moves like a hinge, which allows you to sit, walk, squat, or jump. The knee joint is composed of the femur (thighbone), the tibia (shinbone), and the patella (kneecap). The ends of these 3 bones are covered with articular cartilage which provides a smooth, slippery, surface that protects and cushions the bones. The knee joint is lined by a thin synovial membrane that produces normal joint fluid that lubricates the knee.
There are many different types of arthritis that can affect the knee, but the most common ones are osteoarthritis, rheumatoid, and post-traumatic arthritis. Osteoarthritis (OA) is the “wear and tear” type of arthritis. The incidence of OA increases with age. As the cartilage wears away, the protective layer lining the bones decreases. Eventually, this can lead to “bone-on-bone” arthritis. Rheumatoid arthritis (RA) is a chronic, autoimmune disease that attacks multiple joints throughout the body, including the knee joint. In RA, the synovial membrane swells, causing pain and stiffness in the knees. Any previous injury to the knee (fracture, meniscal, or ligamentous injury) may cause instability and additional stress on the knee, thus leading to arthritis over time.
Arthritis of the knee may present as pain and swelling. Patients may notice locking, grinding, popping, or buckling of the knee. Your doctor will need a thorough history and examination. X-rays, particularly in the weight-bearing position, are helpful in making the diagnosis. Further testing with CT, MRI, or bone scan may be needed to rule out other causes of knee pain.
As there is no cure for arthritis, treatment is aimed at relieving symptoms. Lifestyle changes (weight loss & activity modification) can help relieve pain. Physical Therapy & assistive devices for walking can be beneficial as well. Over-the-counter medications may be helpful, but should be discussed with your doctor as some can cause serious side effects. COX-2 inhibitor is a special type of non-steroidal anti-inflammatory drug (NSAID) that may cause fewer gastrointestinal side effects than OTC NSAIDs (Advil, Motrin, Aleve). Prescription strength topical anti-inflammatory medications, such as Voltaren gel or Pennsaid, are also very effective for pain relief and have lower risk of side effects.
Corticosteroids are powerful anti-inflammatory medications that can be injected into the knee joint. These injections help to reduce inflammation and thus provide pain relief. Corticosteroid injections are limited to 3-4 injections per joint per year as excessive injections can be detrimental to the joint.
Patients with rheumatoid arthritis may benefit from Disease Modifying Anti-Rheumatic Drugs (DMARDs). These include methotrexate, sulfasalazine, & hydroxychloroquine. Biologic DMARDs such as etanercept (Enbrel) & adalimumab (Humira) may dampen the hyperactive immune response. DMARDs are managed by a rheumatologist as there are many options available & several different forms of arthritis that will require long-term follow-up care.
Viscosupplementation is another option for patients with OA. This involves injections of hyaluronic acid supplements into the knee joint which have become known as “gel” or “rooster comb” injections. Various brands of hyaluronic acid are available, such as Euflexxa, Synvisc, or Hyalgan, some of which are derived from the rooster’s comb. In the healthy knee joint, hyaluronic acid acts as a shock absorber and lubricant, allowing a smooth gliding motion at the knee. The hyaluronic acid supplement is thought to improve the quality of the synovial fluid of the arthritic knee & therefore improve shock absorption, decrease inflammation, & improve pain. Depending on the brand, viscosupplementation can be completed in 1 injection or may require 3-5 weekly injections. Viscosupplementation may be effective for 6 months & can be repeated every 6 months if necessary.
Non-surgical management of arthritis of the knee can be successful for years or decades. However, when the knee pain fails to respond to these treatments, surgical treatment may be recommended. Surgical options include osteotomy, partial, or total knee replacement.
Fracture Care
Bones may break (fracture) if they encounter trauma. These fractures may be small, requiring only some protection for healing or they may be larger and more significant, sometimes requiring surgery.
If a fracture places a bone out of proper alignment, your surgeon will likely perform a reduction or “set” the bone. Many times, a cast is the only needed protection afterwards. Your surgeon will likely want to see you several times before the cast is removed in order to check x-rays to be certain the fracture remains in good position. As a general rule, fractures require at least 6 weeks to heal.
Many fractures cannot be set without actually performing surgery and placing metal plates and screws or other devices in order to hold the fracture in good position. This is called open reduction internal fixation (ORIF). Your surgeon will counsel you as far as the best method to treat your fracture. Most of the time, the metal implants will not need to be removed unless they become bothersome for the patient.
Close follow-up care is also an important part of full recovery after a fracture. Many times, physical therapy is helpful in regaining range of motion, strength and function. Your surgeon will be able to determine if you require therapy after your fracture has healed.
Ready to Talk?
Contact Us